LONG COVID by Chikal A. Patel, M.D
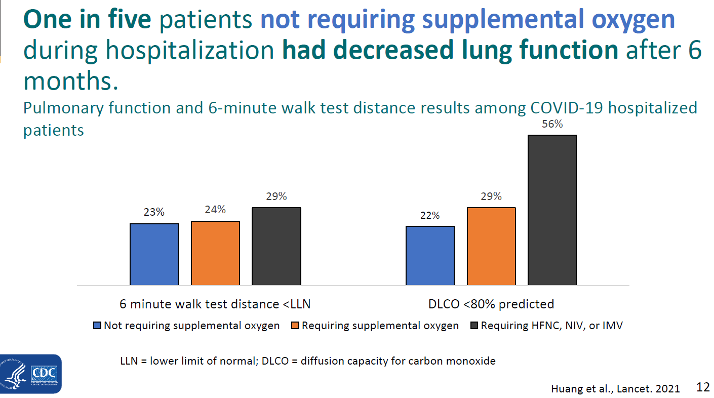
In a 6-month follow-up cohort study, Huang et al. followed 733 patients after hospital discharge. Those with more severe illness during hospital stay tended to have more severe impaired pulmonary diffusion capacities and abnormal chest imaging manifestation. Of additional concern, 1 in 5 patients who did not require supplemental oxygen during hospitalization had reduced lung function 6 months after "recovery."
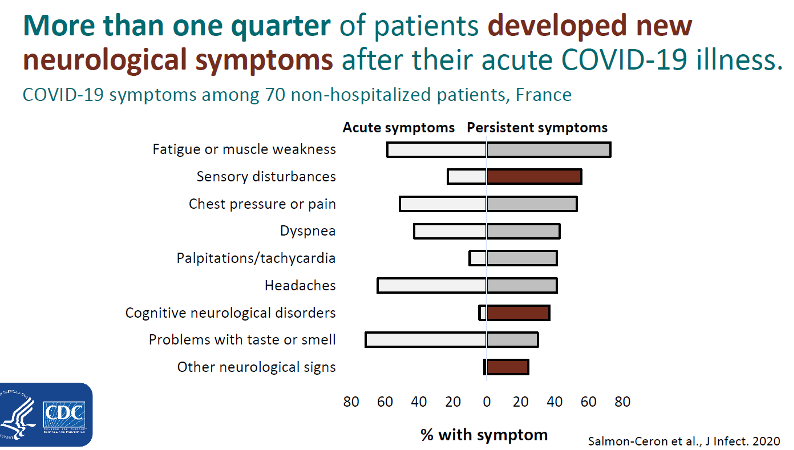
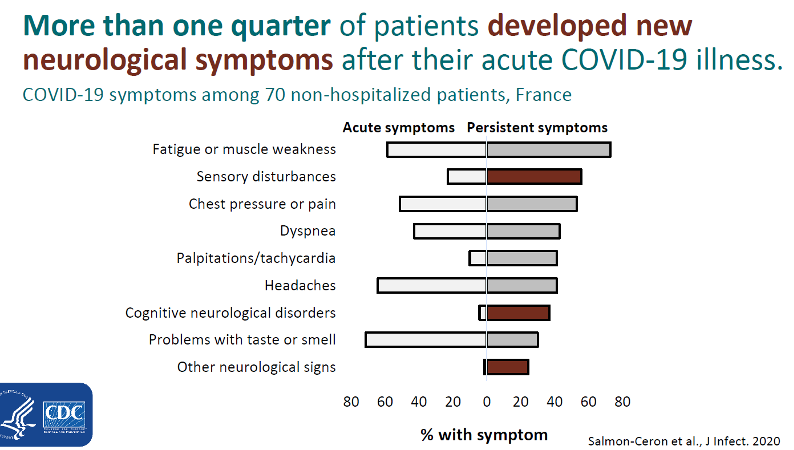
Of the 1,733 patients followed by Huang et al, 76% had at least one ongoing symptom 6-months after initial COVID-19 diagnosis. Among 70 non-hospitalized patients in France, Salmon-Ceron et al pointed out that while many patients had persistent symptoms of fatigue, muscle weakness, chest pressure, dyspnea, tachycardia and problems with taste and smell, more than ¼ of patients developed new neurological symptoms AFTER their acute COVID-19 illness resolved. These findings of decreased lung function 6 months after diagnosis and new neurologic symptoms after acute illness prompt the need for continued post-COVID-19 monitoring for lung dysfunction or new neurologic symptoms.
Assessment/Management of Long-COVID
Not much is understood regarding this condition and more studies are needed. Things you can do as a clinician:
- Be aware of it
- Be empathetic
- Baseline and serial comprehensive reviews of systems and physical exams may better document possible long COVID manifestations
- Symptomatic and supportive care for most symptoms, esp. neurological
- Address and readdress goals of care conversations
Additional information on Long-COVID-19
COCA Crisis Standards of Care (cdc.gov) – Long COVID-19 Presentation from 1/28/21
Late Sequelae of COVID-19 | CDC – CDC update as of November 2020 on COVID-19 Late Sequelae